Our incredible microbiota is a vastly complex community comprised of trillions of bacteria and yeasts.
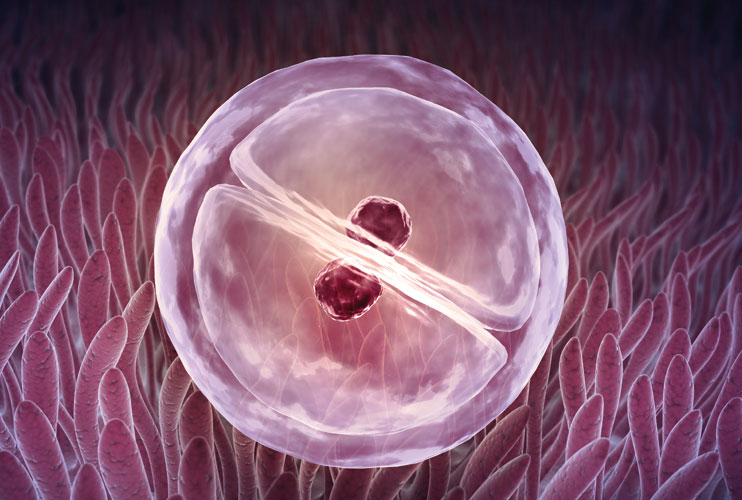
Our gut microbiome has been extensively studied over recent years, though it’s still slightly less common to hear about our reproductive microbiome – male and female. This is a fascinating area of research and one which had led to breakthroughs for my fertility clients, often revealing previously unknown reasons why conception may not have occurred.
When I first begin working with couples preparing for pregnancy, I ask them what their priorities are. The most common answer initially is ‘to have a baby’. To support this aim we need to go a little further and look at what’s happening with crucial structures and processes in the body.
Introducing the reproductive microbiome
Nutrition for fertility involves a good look at the health of our microbiome. If there are any gut, vaginal or skin symptoms this is often a sign that the galaxies of microbes that live in our body may have shifted towards the less helpful or even potentially harmful. When this occurs, they may not be working in our best interests or creating the best environment for creating a new life.
Though the world of these tiny invisible organisms is one we are only beginning to explore, nutrition offers us practical ways of bringing back a harmony which may support our goal of pregnancy and a healthy child.
1/ Your stress levels may compromise your gut health and fertility status
Even under the best of circumstances, the process of childbirth and raising a healthy family could be compared to running a marathon. We can prepare ourselves mentally and physically in the same way. For many of us this road is long and even potentially traumatic with loss and grief along the way. One of the most unfortunate ironies of pre-conception nutrition is the amount of stress involved and also the potential for stress to negatively impact your fertility status.
Reducing your stress levels and cultivating positive stress management techniques may have the potential to improve your fertility status[i]. One reason for this may be due to the changes to the microbiome that occur when we are chronically stressed. Just as our gut bacteria may affect the way our brain works and our stress response, so our stress levels may negatively affect the health of our microbiome.
For this reason, we focus on positive stress management as well as the health of our microbiota in an effective pre-conception programme.
2/ Unhelpful microbes may negatively impact sperm health
In a study examining the seminal fluid microbiota and semen quality the authors found that the quality of the male microbiome may influence the health of semen. Prevotella were found in lower quality semen while Lactobacillus were predominantly found in 80.6% of normal semen samples[ii].
3/ An altered female microbiome may compromise your fertility status
Bacterial Vaginosis (BV) is the most common vaginal condition affecting women during reproductive age and it’s bad news for fertility.
BV is associated with infertility, inflammation in the inner lining of the uterus, pelvic inflammatory disease, late foetal loss, preterm birth, preclinical pregnancy loss – potentially due to uterine receptivity as opposed to embryo quality in in vitro fertilization (IVF) embryo transfer (ET).
BV is a polymicrobial condition describing the health of the vaginal microbiome. Often involving Gardnerella vaginalis though there are other microbes identified as contributing to upper and lower female reproductive tract imbalance. Advances in testing mean that we now have the capability to assess the intimate female microbiome.
4/ A healthy female microbiome may support your fertility
Healthy levels of lactobacilli may support successful implantation and pregnancy, either via Assisted reproductive technology (ART) or natural childbirth[iii]
Our microbiome may offer a hospitable supportive environment to a newly conceived child or it could be less hospitable. Supporting the microbiome before conception helps to rebalance your microbe population in favour of the more beneficial microbiota, ensuring less of those which could potentially negatively impact fertility, conception and the health of your child.
Additionally, an altered vaginal microbiota may affect childbirth. Pathogens we have identified which are thought to cause subclinical changes include Mycoplasma tuberculosis, Chlamydia trachomatis and Neisseria gonorrhoeae.
These changes may be risk factors for subfertility and so in addition to standard testing for sexually transmitted diseases (STDs), investigations into the vaginal flora may reveal altered microbiota as well as altered terrain and pH, potentially useful when preparing for a pregnancy or for Assisted Reproductive Technology.
A 2014 study demonstrated the potential benefits of vaginal colonization with L. crispatus, commonly thought to be the key strain for fertility. This IVF study involving healthy women showed promising results after vaginal colonization with L. crispatus[iv]
5/ Having your inflammation under control is crucial for a healthy pregnancy
Having a predominance of less helpful bacteria in your gut and reproductive tract goes hand in hand with inflammation. Conversely, our beneficial bacteria produce short chain fatty acids which have the potential to reduce inflammation and modulate the immune system.
The early stages of pregnancy involve immune signals which depend on the favourableness of the microenvironment. The quality of the environment has the potential to profoundly alter pregnancy outcome. The cytokine network is therefore an important part of conception and implantation. Inflammatory processes may negatively affect implantation and foetal and placental development[v]
Environmental factors such as stress, nutrition, obesity, chemical toxins, pharmaceutical drugs and high or excessive alcohol consumption may negatively influence the reproductive tract microbiome and subsequently the developing embryo and inflammatory environment[vi]
An opportunity to improve our health while we prepare for pregnancy
The gut microbiome and the reproductive microbiome in men and women are relatively new though potentially revolutionary areas of research for fertility.
One of the reasons I’m so passionate about nutrition and lifestyle medicine is that it gives us a way of addressing imbalances at the root. What happens then may be transformative in many ways depending on the unique individual and their particular genetics and microorganism populations.
If you suspect you may be experiencing any of the conditions mentioned in this article please work with your medical provider as well as your nutritional therapist to ensure you receive the best standard of care.
For further information on working with Eli Sarre or booking a consultation please contact us
Eli Sarre MA MA DipNT mBANT CNHC
Founder of Wildfare and Nutritional Therapist
References and acknowledgements
[i] Sharma R, Biedenharn KR, Fedor JM, Agarwal A. Lifestyle factors and reproductive health: taking control of your fertility. Reprod Biol Endocrinol. 2013;11:66. Published 2013 Jul 16. doi:10.1186/1477-7827-11-66
[ii] Weng SL, Chiu CM, Lin FM, et al. Bacterial communities in semen from men of infertile couples: metagenomic sequencing reveals relationships of seminal microbiota to semen quality. PLoS One. 2014;9(10):e110152. Published 2014 Oct 23. doi:10.1371/journal.pone.0110152
[iii] Hyman RW, Herndon CN, Jiang H, et al. The dynamics of the vaginal microbiome during infertility therapy with in vitro fertilization-embryo transfer. J Assist Reprod Genet. 2012; 29(2):105–115. [PubMed: 22222853]
[iv] Sirota I, Zarek SM, Segars JH. Potential influence of the microbiome on infertility and assisted reproductive technology. Semin Reprod Med. 2014;32(1):35–42. doi:10.1055/s-0033-1361821
[v] Robertson SA, Chin PY, Glynn DJ, Thompson JG. Peri-conceptual cytokines—setting the trajectory for embryo implantation, pregnancy and beyond. Am J Reprod Immunol. 2011;66(Suppl 1):2–10. [PubMed: 21726333]
[vi] Piccinini AM, Midwood KS. DAMPening inflammation by modulating TLR signalling. Mediators Inflamm. 2010; 2010